Special Report: Engineering the Future of Surgery
Collaborations between engineers and surgeons in the UC San Diego Institute of Engineering in Medicine are helping to drive the next generation of medical care. This story looks at three recent collaborations: one aimed at developing a treatment for pancreatic cancer; another focused on ensuring telesurgery can be done safely and efficiently; and a training course in which engineering students shadow physicians as they visit patients, perform surgeries and diagnose disease.
February 7, 2019 | By Liezel Labois and Lindsay Morgan
Engineers and surgeons may not seem at first blush to be the most natural of partners—engineers work in labs, devising and creating new structures and systems, while surgeons work with sick patients and perform repairs on the human body. But when they join forces, these disciplines have the potential to produce technological advances that help patients live longer, healthier lives.
At the University of California San Diego, engineers and surgeons work together both in the lab and in the classroom on a broad array of medical innovations. They are re-engineering white blood cells to treat pancreatic cancer; developing augmented reality systems that could allow surgeons to remotely operate on patients in distant locations; and creating 3D modeling tools to help surgeons plan out the best surgical procedures before operating on patients.
A key catalyst behind these collaborations is the university’s Institute of Engineering in Medicine (IEM), which recently celebrated its 10th anniversary. Since its launch in 2008, the IEM has been connecting engineers and physicians with the goal of improving health care delivery through next-generation tools and technologies.
 “The Institute is a campus-wide initiative to synergize our unique strengths in engineering and medicine—two fields in which we have top-ranking faculty and resources at UC San Diego,” says Shu Chien, MD, PhD, Professor of Bioengineering and Medicine, and founding Director of the IEM. “By applying engineering principles and technologies to the study of medicine, our researchers are generating innovative approaches to diagnose, treat and prevent diseases.”
“The Institute is a campus-wide initiative to synergize our unique strengths in engineering and medicine—two fields in which we have top-ranking faculty and resources at UC San Diego,” says Shu Chien, MD, PhD, Professor of Bioengineering and Medicine, and founding Director of the IEM. “By applying engineering principles and technologies to the study of medicine, our researchers are generating innovative approaches to diagnose, treat and prevent diseases.”
A subset of these innovations involves collaborations between the Jacobs School of Engineering and the Department of Surgery at UC San Diego. Building on the university’s long tradition of interdisciplinary research, scientists from both disciplines are working together to improve clinical medicine and transform patient care.
Programming White Blood Cells to Fight Cancer
 Michael Bouvet, MD, Professor of Surgery in the Division of Surgical Oncology, who specializes in endocrine surgery, has been working with Peter Wang, PhD, Professor of Bioengineering, to develop a treatment for pancreatic cancer, one of the most lethal forms of human cancer.
Michael Bouvet, MD, Professor of Surgery in the Division of Surgical Oncology, who specializes in endocrine surgery, has been working with Peter Wang, PhD, Professor of Bioengineering, to develop a treatment for pancreatic cancer, one of the most lethal forms of human cancer.
 “It’s very difficult to cure pancreatic cancer. Often times the tumors escape and spread and patient survival is very poor. So we’re looking for better ways to treat patients and we want to make them more specific for patients’ tumors to ensure higher chances of success,” says Bouvet.
“It’s very difficult to cure pancreatic cancer. Often times the tumors escape and spread and patient survival is very poor. So we’re looking for better ways to treat patients and we want to make them more specific for patients’ tumors to ensure higher chances of success,” says Bouvet.
Bouvet and Wang’s approach involves reprogramming a type of white blood cell, called monocytes, to target and eradicate pancreatic cancer tumors. Wang’s team is developing a way to genetically modify monocytes so that they target pancreatic cancer cells, and then upon hitting their target, transform into another type of white blood cell, called macrophages, which are able to essentially eat and destroy cancer cells. Bouvet’s team then tests these re-engineered monocytes in mouse models of pancreatic cancer. The work is currently at the proof of concept stage. Results from mouse studies are preliminary but promising.
Wang notes how invaluable it is for engineering teams to have clinical partners to help steer and fine tune their ideas.
“As engineers, we can come up with ideas from our imagination and we want to see if they will work in the lab at all. But clinicians can provide a more practical point of view of what will work in the body, what’s safe,” says Wang.
Overcoming Delays in Long-Distance Surgery
Another engineering-surgery team is tackling a different kind of problem—extending the reach of surgeons by allowing them to operate remotely on patients located across a city, country, or even the globe. This feat can be made possible with a technology called telesurgery. Telesurgery is not performed today, but is a promising goal for the future. Researchers are working to ensure that telesurgery can be done safely and efficiently.
Having the capability to perform remote telesurgery would open up several new realms of patient care. For example, it would allow patients in remote locations greater access to specialized surgeons, creating the possibility of collaborative multi-surgeon and multi-institutional operations, and even bringing surgical care to the front lines of acute trauma situations.
The major hurdle that stands in the way of realizing telesurgery is the signal delay when transmitting commands from a surgeon’s console to the robot at the patient’s bedside, and the video back to the surgeon.
 “We can’t do surgery at long distances right now because there’s a delay when we try to command robots at another physical location. The delay confuses surgeons, it makes it hard to control things,” says Ryan Orosco, MD, Assistant Professor of Surgery in the Division of Head and Neck Surgery Oncology. “The signal delay is unavoidable, so we need creative engineering solutions to combat its effects.”
“We can’t do surgery at long distances right now because there’s a delay when we try to command robots at another physical location. The delay confuses surgeons, it makes it hard to control things,” says Ryan Orosco, MD, Assistant Professor of Surgery in the Division of Head and Neck Surgery Oncology. “The signal delay is unavoidable, so we need creative engineering solutions to combat its effects.”
The delay is similar to turning on the shower and waiting for the water to warm up, explains Michael Yip, PhD, Assistant Professor of Electrical and Computer Engineering. “You have to wait a few seconds before you get the water to reach the right temperature. But imagine having to do this over and over for several hours—that’s what makes telesurgery impossible to do.”
 Yip and Orosco teamed up on a project aimed at overcoming this delay. They are working on augmented reality systems that predict where instruments should go before they are moved and overlay these positions on a screen so a surgeon can observe, in real time, where their instruments essentially are without the effect of delay. The team is also working on visual-haptic feedback that predicts and displays how much force remotely controlled instrument are applying to tissues.
Yip and Orosco teamed up on a project aimed at overcoming this delay. They are working on augmented reality systems that predict where instruments should go before they are moved and overlay these positions on a screen so a surgeon can observe, in real time, where their instruments essentially are without the effect of delay. The team is also working on visual-haptic feedback that predicts and displays how much force remotely controlled instrument are applying to tissues.
“Instead of relying on delayed visual feedback to see what actually happened, a surgeon can use augmented reality to predict what will happen and then operate in this predictive space. As the instruments move, the robot carries out the actions a bit later on, but the surgeon doesn’t see that effect. So it will feel a lot more comfortable and it will be significantly faster to do these procedures,” says Yip.
Training Clinical Engineers
The blending of engineering and surgery isn’t just taking place in research labs at UC San Diego, it’s happening in the classroom as well.
The Jacobs School of Engineering offers the “Clinical Bioengineering” course, in which engineering undergraduates shadow physicians, learn about problems in their clinical practice, and develop engineering-based solutions to bridge the gap between the bench and the bedside. In some cases, students have even obtained funding to turn their solutions into reality.
 The Clinical Bioengineering course is taught by Adam Engler, PhD, Professor of Bioengineering. He adapted it from his alma mater, the University of Pennsylvania, where he was part of the first cohort of undergraduate students taking a version of the class. UC San Diego is the second institution in the U.S. to implement a class in which engineering students shadow physicians as they visit patients, perform surgeries and diagnose disease.
The Clinical Bioengineering course is taught by Adam Engler, PhD, Professor of Bioengineering. He adapted it from his alma mater, the University of Pennsylvania, where he was part of the first cohort of undergraduate students taking a version of the class. UC San Diego is the second institution in the U.S. to implement a class in which engineering students shadow physicians as they visit patients, perform surgeries and diagnose disease.
“This class goes a step further than hands-on and gives students the opportunity to identify and work on problems currently affecting physicians. I’ve seen several groups of students really take these problems to heart and run with their ideas to develop actual products,” says Engler. “Engineering students are expanding their toolbox to include problems that we hadn’t previously exposed them to.”
 “It’s great to see how clinical problems can be resolved with their ideas,” says Deborah Watson, MD, Professor of Surgery in the Division of Facial Plastic Surgery, who is one of the clinician mentors for the course.
“It’s great to see how clinical problems can be resolved with their ideas,” says Deborah Watson, MD, Professor of Surgery in the Division of Facial Plastic Surgery, who is one of the clinician mentors for the course.
Watson’s practice involves performing nasal reconstructions to help patients who have difficulty breathing through their nose. To prepare for some of these procedures, she’ll examine CT scans of a patient’s nasal structure and plan out what framework elements need to be modified or removed in order to increase airflow.
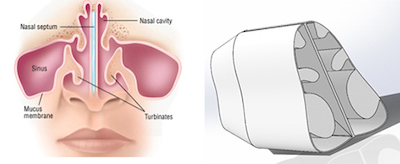 When meeting with students from the Clinical Bioengineering course, Watson would go through these scans in detail and explain how she would make changes to the nasal anatomy and what the resulting airflow would look like. She’d float around an idea—how about designing a way to make patient-specific models of the airspace in the nasal cavity?
When meeting with students from the Clinical Bioengineering course, Watson would go through these scans in detail and explain how she would make changes to the nasal anatomy and what the resulting airflow would look like. She’d float around an idea—how about designing a way to make patient-specific models of the airspace in the nasal cavity?
“The issues with nasal airflow can vary from patient to patient,” says Watson. “With a model of the airway, you could see where some of the narrowing or pinch points have occurred in the nasal cavity and then optimize surgical solutions for each patient to expand those spaces.”
“Seeing all these different airflow passages and how they can change based on the structure inside the nose reminded me of something I’d see in fluid mechanics,” said Stephanie Thomas, a mechanical and aerospace engineering alumna from UC San Diego. “It was a perfect example of something that could be modeled and quantified with physical parameters in order to help surgeons predict how to maximize airflow through a patient’s nose.”
Thomas enrolled in the course because she was interested in applying her mechanical engineering background to medicine. For the final project, Thomas and a classmate, bioengineering alumnus Jonathan Gan, developed a 3D modeling tool to quantify the change in the nasal airflow before and after nasal surgery.
Their tool first creates a 3D digital reconstruction of a patient’s nasal airway passages using CT scans. The user then alters this reconstruction, and the tool uses fluid flow models to show where and how much the airflow had changed.
“This class was a great experience for me as an undergrad and it was really incredible to see how translatable my engineering training was to problem solving in the medical field,” says Thomas. “It speaks a lot about UC San Diego’s commitment to innovation and cross-disciplinary partnerships. Not all universities offer this kind of course and I’m fortunate to have had this amazing opportunity available to me.”
Surgeon-Engineer Match-Making
Challenges remain to remove the roadblocks to surgeon-engineer collaborations. Surgeons and engineers still often work in silos, and although partnerships arise organically, there is no systematized way to match problems with potential solutions.
“Are there ways that we could be doing things differently in order to avoid the silos? We believe there are,” says Andrew Baird, Vice Chair of Research in the Department of Surgery. “The trick is to create a kind of matchmaking environment, where surgeons can say, ‘This is my problem,’ and engineers can in turn say, ‘This is my solution.’”
Match-making is exactly what the Galvanizing Engineering in Medicine (GEM) initiative aims to do. Through the program, clinicians identify an unmet need in patient care and then work with a team of engineers to solve the problem and move the technology to the clinic. Each year, four physician-engineer teams from UC San Diego are selected to receive a GEM award of $60k to help fund their projects. The GEM is a collaboration between the Altman Clinical and Translational Research Institute (ACTRI) and the Institute of Engineering in Medicine, and facilitated by the UC San Diego Office of Research Affairs. The initiative is led by Gary Firestein, Shu Chien and Deborah Spector.
“The GEM program is another way we foster interactions between the two disciplines by bringing engineers and physicians who want to better understand each other’s culture and language together to practice engineering-based translational medicine,” says Chien. “We’re now in the fourth year of this program and have seen many successful teams emerge.”
The latest batch of GEM awardees include Orosco and Yip’s work to address challenges in telerobotic surgery; Bouvet and Wang’s research to treat pancreatic cancer; and a project to develop a next-generation spinal cord neuro-electronic implant to treat paralysis, which includes Department of Surgery faculty Joseph Ciacci, MD, together with Shadi Dayeh, PhD, an Associate Professor of Electrical and Computer Engineering.
Another strategy to create robust engineer-surgeon interactions is to co-appoint School of Engineering faculty directly into the Department of Surgery. To that end, the Department of Surgery is currently in the midst of finalizing two engineering faculty appointments into its Minimally Invasive Surgery and Vasculary & Endovascular Surgery divisions. Dr. Bryan Clary, Chair of the Department of Surgery, suggests that the strategy will further emphasize collaborative research with joint pilot studies and research grant submissions. Says Clary: "The vision of engineering leaders including Juan Lasheras [title] and Geert Schmid-Schonbein [title, check the spelling] have been critical to this approach and from this model we hope to bring additional engineering faculty into the Department."
The Bottom Line
Collaborations between surgeons and engineers at UC San Diego have already produced many awe-inspiring advances in medicine, and the best is yet to come.
“Surgeons and engineers have a lot in common,” says Bouvet. “We want to solve problems and we want to do good for patients. Surgery is becoming ever more technical, and some of the incredible advances we have made are because of the work of engineers. They are critical for improving things in the operating room.”
“It’s about bringing together different points of view with different kinds of expertise. As long as you have two groups that are open-minded, which is the trick, then one and one equals much more than two,” says Baird.
“Looking ahead, we hope to amplify what the IEM has accomplished over the last 10 years and get more physicians and engineers, not just at UC San Diego but at other campuses throughout the nation and throughout the world, to link together and collaborate for the benefit of people’s health. We’re working to make that a reality,” says Chien.
